Conditions & Treatments

Pelvic Organ Prolapse
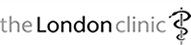
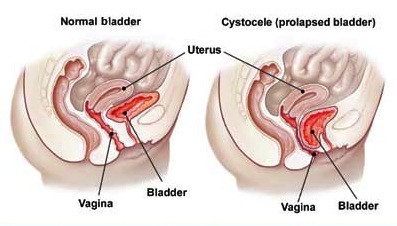
The pelvic organs, such as the womb, rectum and bladder, are held in place by muscles, tissue and ligaments. Prolapse happens when one or more of these organs slips down from its normal position into the vagina, because the supportive tissues have become weak.
Symptoms depend on the organ that has been affected, but prolapse commonly causes:
- A sensation of something coming down or out of the vagina
- An uncomfortable feeling of fullness
- Difficulty having sex
- Leaking a small amount of urine when you cough, sneeze or exercise (stress incontinence)
- Uterine prolapse - the womb pushing through into the vagina
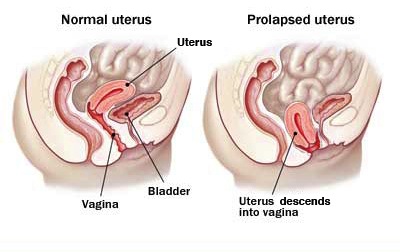
- Enterocele - part of the small bowel pushing through into the vagina
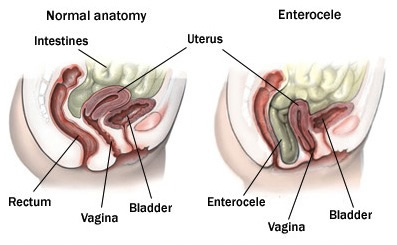
- Rectocele - part of the rectum pushing through into the vagina
- Cystocele - part of the bladder pushing through into the vagina
- Vaginal vault prolapse - the top of the vagina sagging after the removal of the womb (after a hysterectomy)
Who can be affected?
Up to half of all women who have had children are affected by some degree of prolapse. It is more common as women get older, particularly in those who have gone through the menopause. It is rare in women who have not had children.
Prolapse is also associated with being overweight and with having a persistent cough. It is the most common reason for hysterectomy in women aged over 50.
Stages of prolapse
The severity of the prolapse can be determined using the following grading system.
- Stage 1: the prolapse is more than 1cm above the opening of the vagina
- Stage 2: the prolapse is 1cm or less from the opening of the vagina
- Stage 3: the prolapse sticks out of the vagina opening more than 1cm, but not fully
- Stage 4: the full length of the prolapse bulges out of the vagina
How is prolapse treated?
Mild cases of prolapse may not need treatment. Lifestyle changes such as weight loss and pelvic floor exercises may be recommended instead.
More severe cases of prolapse may be treated effectively using a device that is inserted into the vagina called a vaginal pessary. This helps to hold the prolapsed organ in place.
Surgical options include: a repair operation or hysterectomy. Occasionally a mesh can be inserted to support the womb or vagina, in the case of certain types of prolapse, but mesh is generally reserved for repeat surgery.
The impact of surgery on bowel, bladder and sexual function can be unpredictable and may make symptoms worse or result in new symptoms, such as leakage of urine or problems with intercourse.
There are several treatment options available for a pelvic organ prolapse. You will not need any treatment if your prolapse is mild to moderate and not causing any pain or discomfort.
Pelvic floor exercises
Your pelvic floor muscles are the muscles that you use to control the flow of urine from your bladder. They surround the bladder and the tube that carries urine from the bladder to outside the body (urethra). Having weak or damaged pelvic floor muscles can make a prolapse more likely. If you only have a mild prolapse, doing pelvic floor exercises may help to support your prolapse. Exercises will generally not help significant prolapse
Pelvic floor exercises are also used to treat urinary incontinence (when you leak urine), so they can be useful if this is one of your symptoms.
Vaginal pessaries
A vaginal ring pessary is a device that is similar to a diaphragm or cap. It is inserted into your vagina to hold the vaginal walls in place. Ring pessaries are usually made of latex (rubber) or silicone and come in different shapes and sizes. Ring pessaries may be an option if your prolapse is more severe but you would prefer not to have surgery. A gynaecologist (a specialist in treating conditions of the female reproductive system) or a specialist nurse usually fits a pessary. The pessary will be removed every three to six months and replaced with a new one.
Side effects
Ring pessaries can occasionally cause vaginal discharge. They may also cause some irritation and possibly bleeding and sores inside your vagina. Other common side effects include:
- An infection of your urinary tract (urinary tract infection)
- An imbalance of the usual bacteria that are found in your vagina (bacterial vaginosis)
- Passing a small amount of urine when you cough, sneeze or exercise (stress incontinence)
- Difficulty with bowel movements
- Interfering with sex
Surgery
Several different types of surgery can be used to treat a severe genital prolapse. These procedures include:
- Surgery to repair the tissue that supports the prolapsed organ
- Surgery to repair the tissue around the vagina
- Surgery to close the opening of the vagina
- Surgery to remove the womb (hysterectomy)
These procedures are outlined below.
Vaginal Repair
Prolapse of the vaginal wall (not the uterus) is the commonest type of prolapse. This type of prolapse may involve the front wall of the vagina (below the bladder), the back wall (below the rectum) or the top of the vagina (if the uterus has been removed) - called a vault prolapse. The surgery involves reinforcing the weakened area to prevent it from bulging and a mesh maybe considered for repeat surgery if the woman's own tissues have not held together after a first operation. The surgery type is called:
- Anterior Repair
- Posterior Repair
- Vault Repair (Sacrospinous fixation or Abdominal Sacrocolpopexy)
Downloads
- Posterior Vaginal Wall Prolapse Repair And Repair of Perineum
- Suspended Mesh Kit Anterior Prolapse Repair
- Suspended Mesh Kit Posterior / Vault Prolapse Repair
- Operations for Prolapse of the Vaginal Apex
- An Operation for Anterior Vaginal Wall Prolapse
- Sacrocolpopexy for Vault Prolapse
Hysterectomy
A hysterectomy is a major operation that involves removing the womb (uterus). When performed for prolapse it is usually because the womb is protruding out of the vagina or is sitting very low in the vagina. It may be considered as a treatment for some types of pelvic organ prolapse, although there maybe an increased risk of vaginal vault prolapse (where the top of the vagina starts to prolapse). You cannot get pregnant after having a hysterectomy.
Downloads